A Middle-Aged Nurse Dies during Botched Treatment of Back Pain
In August 2018, a 44-year-old registered urgent care nurse who had been diagnosed with chronic back pain died in a suspected case of unintentional (non-suicide) lethal drug overdose, which was classified as combined drug intoxication devoid of alcohol intake. The mother of three worked in Rochdale Infirmary and had just concluded her night shift on that fateful day, and upon reaching home, she took several medications that later caused her to collapse on her kitchen floor.
According to her medical records at the time of her death, she had been prescribed to take 6 different drugs to manage her diagnoses of chronic back pain following a slipped lumbar disc, insomnia, anxiety, and post-natal depression. The prescribed drugs were Diphenylhydramine (Nytol), Pregabalin, Oxycodon, Diazepam, Hydroxyzine, and Flucloxacillin. Her primary care physician admitted that her prescriptions contained strong painkillers – a combination of Oxycodon and Diazepam – to manage flare-ups of her back pain which could at times make walking painful and difficult for her.
Her toxicology report showed the following drugs in her system: Fluoxetine, Diphenylhydramine, Pregabalin, Chlordiazepoxide, Oxycodon, Diazepam, Hydroxyzine, Amitryptline, and Flucloxacillin. The coroner who was involved in recording her death report pointed out that she was most likely driven to take the cocktail of medications because of chronic back pain that could have aggravated her sleeping problems.
Back Pain
The above-mentioned medical incident shows how debilitating back pain can be, especially when it is not managed properly. The media report reveals that the deceased nurse had been diagnosed with lumbar disc disease though it did not mention if she had been advised to use a lumbosacral back support. This lumbar disc disease was caused by herniation of the intervertebral disc in the lumbar spine, which set off acute low back pain. She suffered this back pain for a period of more than 6 months hence its classification as chronic back pain. She may have suffered sciatica which made it painful for her to walk, while possible nerve compression in her lower back may have caused muscle weakness in her thighs and legs which would have made walking difficult.
This case study leads to several basic questions:
- What is back pain?
- How is it diagnosed?
- How is it managed well?
This post will focus on chiropractic care (which is a direct approach to spinal manipulation) and low back pain.
What is Pain?
Pain can best be described as the unpleasant distressing experience that is caused by any noxious stimulus. This description shows that pain has an emotional and sensory aspect to it. The sensory perception is provided by noxious stimuli. The emotional aspect is the distressing experience that normally causes one to withdraw the affected body part from the offending stimuli.
Clinically, any pain is considered a symptom that points to an underlying pathological process that is normally associated with tissue damage. Unrepaired tissue damage results in a disease that can be diagnosed and needs to be managed.
If this pain is experienced in the back, then it is called back pain.
The Lower Back
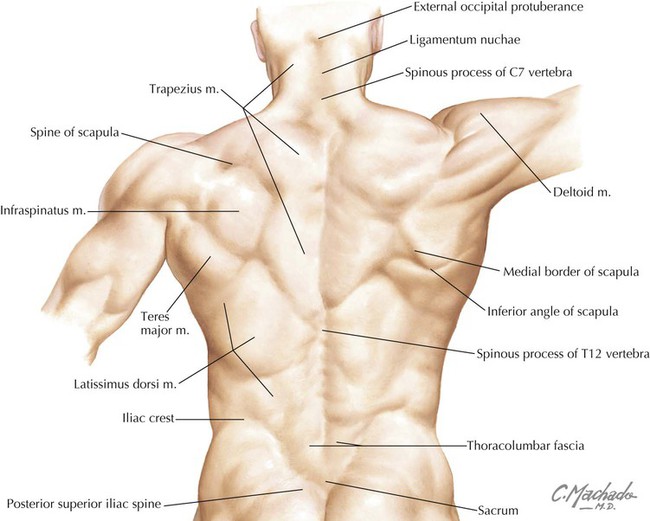
Anatomically, the human back starts at the base of the neck and ends at the top of the gluteal (buttocks) region. The principal bone of the back is the vertebral column (also called the spine), which gives each person the curvature of his/her back.
This vertebral column is divided into 4 anatomically distinctive regions – the cervical, thoracic, lumbar, and sacral spines or vertebrae. The spine is the main axial bone in the human skeleton.
The thoracic spine and lumbar spine form the back-bone i.e the main bone of the back. The lumbar spine forms the lower back, while the thoracic spine forms the upper back. The sacral spine is part of the gluteal region, while the cervical spine is part of the neck region.

Etiology
Back pain is a disease, which means that it is a manifestation of tissue damage. The main causes of back pain in order of frequency are:
1. Sprain and Strain: According to a study done by Manchikanti et al (2009), over 85% of all cases of back pain have a non-specific cause/etiology, though the history of peripheral injury to the muscles and ligaments of the back region is present. This shows the importance of good history taking that lucidly documents the history of presenting illness. For this reason, working with a chiropractor who has formal medical training becomes an advantage because a good medical history exponentially increases the probability of a correct diagnosis. One of the leading causes of sprain and strain of the back is poor posture.
Strain is caused by tears in the muscle fibers that occur when the muscle is overstretched. These tears can also occur in the tendons that connect the muscle to the vertebral column. One of the main causes of overstretching muscles is poor posture. Other causes are strenuous physical exercises and manual work.
Sprain is tearing of ligaments and is usually less common but more painful than strain. A sprain is normally caused by physical trauma to the back.


2. Spinal Disc Herniation: This is an injury that affects the intervertebral disc, and causes its soft core – the nucleus pulposus – to protrude through the fibrous outer ring – the annulus fibrosus. This herniation occurs towards the back of the spinal column because its posterior ligament is weaker than the anterior ligament, and as such, cases of anterior disc herniation are rare with the exception of severe degenerative disease or catastrophic physical trauma that leads to fracture of the spinal column. At times, this intervertebral disc herniation is described as slipped disc, but this term is clinically incorrect though it’s popular as a colloquial term.


Another condition that is confused with disc herniation is disc protrusion. Disc Protrusion occurs when the annulus fibrosus protrudes into the spinal canal and intervertebral foramina (explained later). In disc herniation, the annulus fibrosus is ruptured so that the nucleus pulposus protrudes through, which leads to the release of inflammatory chemicals which explains the inflammatory reaction associated with disc herniation. This protrusion of the nuclues pulposus has led to disc herniation being described as intervertebral disc prolapse and ruptured intervertebral disc. On the other hand, in disc protrusion, the annulus fibrosus is not ruptured hence there is no protrusion of the nuclues pulposus and no inflammatory chemicals are released, which explains why this condition is described as a bulging disc. Unlike disc herniation, disc protrusion is not normally associated with inflammation, though it can cause spinal stenosis, lumbar stenosis, and nerve root compression (explained later).

The presence or absence of inflammation in disc herniation and disc protrusion highlights the need for a professional chiropractor to request both radio-imaging (to visualize the spinal column) and 3 types of blood tests – complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels. Magnetic resonance imaging can help a medically-trained chiropractic to locate inflammation.
Other Causes that cannot be managed by Chiropractic Care: Other causes of low back pain are neoplastic lesions (and cancer), autoimmune diseases like rheumatoid arthritis, infections like an epidural abscess, and degenerative diseases such as spinal stenosis, spondylolisthesis, spondylosis (degenreative arthritis), and pathologic fractures. Pathologic fractures are common among the aged, and the main type of fracture that occurs is vertebral compression fracture (Jarvik, 2002), which is normally associated with a shortening of the physical height of the affected person.
Types of Back Pain
There are 4 main types of back pain:
1. Local Pain: This is pain that occurs when pain receptors in the somatic tissues e.g skin, muscles, ligaments, and tendons are stimulated by noxious stimuli. It is a form of nociceptive pain because it is pain receptors (also called nociceptors) that relay the pain. It is also called somatic pain.
2. Referred Pain: This is pain that is felt away from its source (tissue of origin) i.e the location that one feels the pain is different from the source (location) of the pain. It is also called radiated pain. A Chiropractor cannot manage referred/radiated pain because it is normally caused by disease in the abdominal cavity e.g kidney stones whose pain radiates to the flanks of the lumbar region. Other diseases include bladder infection, pancreatitis, and the potentially mortal abdominal aortic aneurysm. Referred pain is usually a form of visceral pain, which is pain that is associated with damaged internal organs.
3. Radicular Pain: This is local pain in the lumbar spine and surrounding region that is radiated to the thigh and leg muscles that are innervated by nerves that issue from an injured nerve root.
4. Neuropathic Pain: This is pain caused by nerve injury, and can occur during disc herniation, but is rare in muscle strain. It is quite different from nociceptive pain. Radiating pain flares in the thigh region when one tries to pick up an object from the ground, and this is because the nerve root is stretched when one bends forward.
Pain can be graded based on duration into:
- Acute Pain: This is pain that has lasted for less than six (6) weeks.
- Sub-acute Pain: This is pain that has lasted for more than 6 weeks but less than 6 months.
- Chronic Pain: This is pain that has lasted for more than 6 months.
Pain can be described as either dull pain or sharp pain:
- Dull Pain: This is an ache that is tolerable and allows one to go on with daily activities. It normally occurs in sub-acute and chronic pain.
- Sharp Pain: This is excruciating pain that can be described as stabbing, throbbing, intense, or gripping pain. It is associated with acute tissue injury, and as expected, occurs in acute pain. If this sharp pain is associated with neuropathic pain, then it is described as neuralgia.
Disc Herniation, Lordosis, and Lumbar Stenosis
The vertebral column is made up of complex irregular bones called vertebrae. The bodies of two adjacent vertebrae are joined together by special fibrocartilaginous joints called inter-vertebral discs that serve as shock absorbers and allow for very slight movement between them. It is this slight movement permitted by the intervertebral discs that allow chiropractors to perform spinal manipulation, which is critical to managing low back pain that is caused by strains, sprains, and herniated discs (though not all types of disc herniation can be managed by chiropractic as an extreme case of ruptured intervertebral discs require surgical intervention).
The vertebral column has a canal called the vertebral/spinal canal that encases the spinal cord which is the main nervous tissue in the body outside of the brain. This means that any injuries to the vertebral column can affect the spinal cord, which can result in extreme pain, muscle weakness, and even loss of function of the muscle groups innervated by nerves originating from the affected section of the vertebral column.
In the case mentioned above, the nurse suffered a slipped intervertebral disc in the lumbar spine which pressed against her lumbar nerve roots.

There are only 5 vertebrae in the lumbar spine, and they have been conveniently named Lumber 1 (L1) through to Lumber 5 (L5). The L1-L5 lumbar spine gives the back its convex curvature, and if this convexity is beyond the normal limit, then the resulting condition is called lordosis.
Posterior to (behind) each intervertebral disc in the lumbar spine are 2 large open passages called intervertebral foramina that allow nerve roots to pass from the spinal cord to the outside of the vertebral column. Also, each vertebrae has 3 processes (bony projections) for attachment of ligaments and tendons of muscles with the spinous process being the most prominent process.
The nerve roots are the base of nerves that innervate the back muscles, as well as all the muscles in the thighs and legs
If the size of the intervertebral foramen is decreased, the space available for the nerve root to pass through is consequently decreased. This condition is called neural foraminal narrowing and it leads to compression of nerve roots, which is medically designated as nerve root compression. When neural foraminal narrowing occurs in the lumbar spine, it is called lumbar stenosis, and it can cause back pain whose intensity increases sharply when one bends the back, especially bending forward which stretches the back muscles and marginally pulls the nerve roots.

Any injury to the nerve root is called radiculopathy. If the nerve root compression is severe, the affected person can develop weakness and numbness in the thighs and legs, and this is indicative of peripheral neuropathy. At times, this nerve compression causes a sharp shooting pain to travel down the lower back to the thighs and legs, and this form of radicular pain is called sciatica. Sciatica is indicative of existing radiculopathy, which is usually designated as lumbar radiculopathy, sacral radiculopathy, or lumbosacral radiculopathy.
Lumbar stenosis can make walking and maintenance of balance (during walking) difficult. This is quite prominent if the neural foraminal stenosis occurs in both the right and left intervertebral foramina as is the case in disc herniation.
In the aforementioned case, the nurse had lumbar stenosis which led to nerve root compression, hence her chronic low back pain and difficulty in walking. Among the drugs prescribed to the late nurse were tricyclic antidepressants. Some of the tricyclic antidepressants which are known to have a beneficial effect in managing chronic low back pain are pregabalin, gabapentin, amitriptyline, doxepin, desipramine, nortriptyline, clomipramine, protriptyline, and imipramine. Other antidepressants that can be used are bupropion, duloxetine, and venlafaxine.
According to Ward (1986), desipramine – a non-sedating antidepressant – caused significant pain relief in 60% of the patients with chronic low back pain who took the drug. This efficacy is almost equivalent to the efficacy of doxepin (ibid). However, a meta-analysis study done by Salerno, Browning, & Jackson, and published in 2002 revealed that antidepressants can help relieve low back pain but cannot improve the functional status of a patient suffering from chronic low back pain. For this reason, pharmacotherapy (i.e drug-based treatment) must be augmented by physical therapy and/or spinal manipulation so as to improve the functional status of the patient.
A key demerit of poly-pharmacy (i.e taking multiple drugs at the same time) is the risk of adverse drug interactions. Drug interactions are the reactions between 2 or more drugs that take place in the body, and can cause the drugs to lose their clinical efficacy or potentiate the adverse effects of the reacting drugs. Drug-to-drug reactions that lead to death are described as lethal drug interactions. An example of lethal drug interaction is the use of benzodiazepines, cocaine, or opiate analgesics after taking alcohol because it leads to a decrease in breathing rate (a condition called hypoventilation) that can result in respiratory failure and ultimately death.
A professional chiropractor should be able to take a comprehensive medical history that includes a history of drug use and compliance with prescription medications. This will allow for a benefit-to-harm evaluation of whether some drugs should be discontinued, or chiropractic care should be avoided, or chiropractic care can be used alongside the prescribed drug regimen. It is for this reason that one is advised to look for an experienced chiropractor who has formal medical training and is licensed to practice by an official licensing board. One of the leading professional chiropractors who has been licensed to practice family medicine is Dr.Eric Wruck.
Diagnosis
The main ways to diagnose low back pain are taking a good medical history, performing a good physical examination (that includes the straight leg test to determine if sciatica is present), and requesting the following diagnostic tests:
1. Radio-imaging: X-ray or MRI (with the costly MRI being able to differentiate between disc protrusion and disc herniation).
2. Blood Tests: CBC, ESR, and C-Reactive Protein levels. In disc herniation, the ESR, white blood cell count, and C-reactive protein levels are elevated (beyond the upper normal limit), while their levels can be normal in disc protrusion.
Management
The World Health Organization recommends the use of analgesics (painkillers) or alternative treatments like spinal manipulation (i.e chiropractic) and physical therapy, as the first line of treatment for low back pain. If this fails, then the next course of action is surgical intervention, especially herniated disc surgery, which can be intervertebral discectomy or intervertebral disc arthroplasty. According to Furunes et al (2017), intervertebral disc arthroplasty is recommended for patients with chronic low back pain who cannot respond to conservative management, and the reason for this approach is that it results in significant long-term improvement in the quality of life of these patients.
Interestingly, the World Health Organization has praised a study done by the World Vertebrology Foundation that concluded that intervertebral discs can self-regenerate if they are subjected to non-invasive decompression, which can be one of the reasons why it has classified physical therapy and spinal manipulation as an alternative first line of management.
According to Dr.Erick Wruck, the best first line of management of chronic low back pain is a complementary therapy that combines chiropractic care with the use of safe non-opioid analgesics. In a consensus process study done by Vining et al (2019), multi-modal chiropractic management of low back pain resulted in clinical pain alleviation if the etiology of the condition is a sprain, strain, lumbar radiculopathy, intervertebral disc protrusion, or bulging (herniated) lumbar intervertebral disc that does not require surgical intervention.
***************
If you live in Hawaii and need professional chiropractic care for managing low back pain, the best clinic that can meet your health-care needs is Back in Action Chiropractic, which is managed by Dr.Eric Wruck (DC, APRN, FNP) in Kahului, Maui. Alternatively, you can reach the clinic at 808-873-0733 or make an appointment by dialing 808-572-6223.
As it has been noted, a professional chiropractor can help manage chronic low back pain, lordosis, sciatica, and as well as help alleviate lumbar stenosis (neural foraminal stenosis) caused by disc herniation.
———————————————
Resources
Furunes, H., Storheim, K., Brox, J. I., Johnsen, L. G., Skouen, J. S., Franssen, E., … & Hellum, C. (2017). Total disc replacement versus multidisciplinary rehabilitation in patients with chronic low back pain and degenerative discs: 8-year follow-up of a randomized controlled multicenter trial. The Spine Journal, 17(10), 1480-1488.
Harrison, T. R., & Jameson, J. L. (2018). Harrison’s Principles of Internal Medicine| Principles of Internal Medicine. McGraw-Hill Education.
Jarvik, J. G., & Deyo, R. A. (2002). Diagnostic evaluation of low back pain with emphasis on imaging. Annals of internal medicine, 137(7), 586-597. (Download Link).
Manchikanti, L., Singh, V., Datta, S., Cohen, S. P., & Hirsch, J. A. (2009). Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain physician, 12(4), E35-70. (Download Link).
Moore, K. L., & Dalley, A. F. (2018). Clinically oriented anatomy. Wolters Kluwer India Pvt Ltd.
O’brien, Zoie. (August 9, 2018). Mother-of-three NHS nurse, 44, given six different drugs to treat her bad back accidentally kills herself with lethal overdose. DailyMail MailOnline.
Raja, S. N., Carr, D. B., Cohen, M., Finnerup, N. B., Flor, H., Gibson, S., … & Vader, K. (2020). The revised IASP definition of pain: Concepts, challenges, and compromises. Pain, 161(9), 1976.
Salerno, S. M., Browning, R., & Jackson, J. L. (2002). The effect of antidepressant treatment on chronic back pain: a meta-analysis. Archives of Internal Medicine, 162(1), 19-24.
Ward, N. G. (1986). Tricyclic antidepressants for chronic low-back pain. Mechanisms of action and predictors of response. Spine, 11(7), 661-665.
World Health Organization. (2020). Priority diseases and reasons for inclusion. Chapter 6.24-Low Back Pain. (Download Resource)
Vining, R. D., Shannon, Z. K., Salsbury, S. A., Corber, L., Minkalis, A. L., & Goertz, C. M. (2019). Development of a clinical decision aid for chiropractic management of common conditions causing low back pain in veterans: Results of a consensus process. Journal of manipulative and physiological therapeutics, 42(9), 677-693.

